Last night while talking to the Dr. He mentioned my sons grade 4 IHV and his grade 2 on the other side.
I told him he only has a grade 4 from what I have seen.
Another phone call this morning.
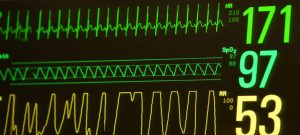
Throughout the night his oxygen percent needs were around mid to High 60’s.
This morning his primary nurse was off going and the same one from yesterday came on shift.
The nurse tells me over the last few hours his needs went up to 100% oxygen.
They suctioned him “really good” not that they don’t always do a good job. Added nitric oxide, and upped his HZ on the oscillator to 12 from 10. Now his oxygen is back down to 57%. So it seems to be working.
Yesterday we were told Nitric oxide would likely not be effective. So I asked if they were both changed at the same time. And they were.
So we don’t know which one is helping. But they tried turning down the HZ and he started desatting so then they put it back up.
I accidentally said nitrous oxide while asking a question and the nurse promptly correct me, nitrous oxide is for cars.
Dr. Comes by. We have a cranial ultrasound sheduled. There seems to be confusion as to if RT has a new brain bleed, an old brain bleed that happened, or what they saw on the ultrasound last Thursday.
How can we have this type of confusion at this point is extremely concerning.
We discuss his increased needs, I ask what the plan moving forward is concerning his ventilator and which one is the correct tool. I tell her I’m not pushing for a particular vent but want what is best. She tells me she will talk to the respiratory tech.
We don’t know which one is best for the little guy.
A short while later the respiratory tech comes pushing in the NIV NAVA machine. Looks like we are switching back to SIMV mode on the conventional ventilator.
He is disconnected from the oscillator and bagged while connecting to the traditional ventilator.
The respiratory tech adjusts the depth of his ventilator tube .5 deeper.
He is back on the machine we were first using now.
I ask if we will get an X-ray to check the depth of his tube.
I am told it’s not needed. Likely just an X-ray tomorrow.
I thought any time a vent tubes depth is changed we have an X-ray.
The nurse and respiratory tech tell me we shouldent need it.
They ask if he likes his tummy. I tell them it’s one of his favorite ways to be positioned usually. They rotate him to his belly.
I ask if they do suction normally after repositioning.
They say no but do it anyways. She gets nothing out.
The Dr. comes in to see how everything has been going. They tell her they can’t wean him down. He just de-sats.
The Dr. tells them she will order an X-ray to insure tube placement is correct. They both agree this is a good idea…
Eventually X-ray shows up. They reposition him to his back for the X-ray. He does well, I look at the X-ray after tech takes it. To me it looks better, not whited out like it was. We will see what they say.
I change his diaper, and clean his eyes. His eyes are still stuck shut.
They rotate him back to his tummy. This time he gets suctioned without me asking, some fluid comes out.
He did well with cares.
This nurse seems to have little faith in RT.
We need someone that believes he can pull through. That loves him, that believes he can.
He begins to trend towards desatting more.
I ask if it would be worth trying suction. She tells me no. This is because of his PDA.
Instead his oxygen percent has been getting turned up.
See he is 97 spo2 now.
I ask again “so it’s not worth trying. To possibly have him do better on a lower percent of oxygen?”
“No suction doesn’t come without drawbacks”
Now his oxygen is turned up to 78%
Day is far from over.
Keep on breathing little man.

Hang in there! SH
LikeLiked by 1 person