Ongoing discussion of when we will potentially be discharged.
The Dr. Says potentially in a weekish… Woah that is soon.
Dr. Is amazed with him.
Pulmonologist is amazed with him.
Surgeons are amazed with him. No one expected him to progress like he has.
He just continues to blow everyone away!
There are some appointments that need to happen first and we need to reach a point where we don’t have to have appointments for a good amount of time. Because we will be driving across the county.
Ultrasound comes and does a echo cardiogram, to make sure hisheart isdoing good still after his heart surgery, last echo was difficult because he was so mad. RT hardly wakes up for it today, the ultrasound tech running the machine is blown away with how well he deals with it. He smiles at her too, she holds the wand much more gently than some of the other ultrasound techs have done. RT appreciates it and shows it! It goes quick. Not one single cry.
One of the appointments earliest it could be scheduled is the 20th for his swallow study. Where they do a live xray add he swallows a radioactive fluid that shows up. Should be cool to see!
The Pulmonologist decides that today is the day.
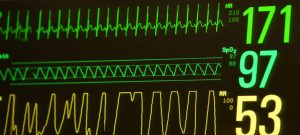
They turn off his oxygen support to see how he does.
15 minutes He is tolerating it great! They remove his nasal prongs.
RT’s face has only stickers on it to hold the prongs in place still incase he needs it back.
He won’t. He doesn’t, not for now!
Eventally the stickers are removed.
Nothing on his face, first time in 145 long days and his face is absolutely freeeeeee! No feeding tube taped to it or anything!
Woah!
We will be practicing feeding today! Starting with a small amount.
With the therapist doing it for now to be extra safe.
RT ends up not waking up at all during cares and does not suck on his binky. Too asleep.
Well it would not be safe to try and feed right now.
For some reason force feeding sleeping babies that have never had to drink before is frowned uppon.
Rescheduled for tomorrow morning 0830. Nice and early. Maybe he will be awake then.
Stable afternoon, especially considering he is now on no support and minimal monitoring spo2 only!
2000 he poops. Change is uneventful, runny like last time, likely because non fortified.
2030 he gets extremely hungry, I try and calm him with his binky and holding. Calm him down for a bit.
2100 his first fortified feed stated Similac TC again. 26 cal.
3/4 of the way through his hour long feed he finally starts to feel full and falls asleep.
2200 60 of his 70 cc feed in and the nurse comes to swap the syringe to give him his last 10CC.
I’m sitting infront of him he’s laying on his side in his bed asleep, and he regurgitated a small river of fortified milk down his cheek. I look up at his spo2 number, still sitting at 99! It looks like he is not fazed by it! Me. … not so much, small internal panick attack begin.
I tell the nurse, she stops his feed.
She goes to tell our nurse. He does it again.
I know all babies have reflux, it is just a matter of how well they deal with it.
A month and a half ago I was told reflux and inhaling it into his lungs was the reason we were re intubated. So yes it’s scary.
We are at a much different place now though, back then he was on 30 cal, cpap of 7 which makes it impossible to swallow, and still premature. All things that make it more difficult to deal with reflux.
But now we are on no oxygen support, after full term. Over a month old corrected gestation. But we know his left vocal cord might be paralyzed and not be able to protect his airway. Much different situation but still terrifying.
The nurse paged the doctor.
He comes and asks if I have any questions, I tell him n what happened.
I know babies all do it, it is a matter of how they deal with it. Back a month and a half ago this is what sent us back so far. We are in a much different place I explain how, and why. Back then I would ask for an xray but this time RT didn’t brady, didn’t desat. He isn’t breathing harder or showing any signs of any issues. So now I don’t know what to ask for.
This is his first fortified feeding since surgery, do we need to stop it and only do plain milk? He tolerated it before surgery. Or since he showed us he dealt with it ok do we do nothing. I think I need to have faith he is more like a normal baby now
He agrees with everything I say. Then says yes we continue unless he shows us he keeps doing it or starts to have an issue.
I’m ok with this, I have to have faith that he can now handle this. He can do this, he has his lucky fin. He showed us he can do it on no oxygen support and not desat in his sleep.
Most people can laugh when a baby vomits. No harm done.
For us it could mean aspiration and fluid into the lungs pneumonia, or even death. Before RT it never really seemed that dangerous. Sure you make sure the baby spits it out, doesnt drown in a puddle of it by being on their belly, flip them from their back onto their side to let it run out etc.
But there is so much going on on the inside you can’t see if there Is a bunch going the wrong way not coming out.
It’s not a haha, its an oh F#€/\€%/€\\\ explative!
We will keep close track of it and if it keeps happening or causes issues we will address it again but for now. Everything is ok.
I’m sure I forgot something but I think I hit the important parts.
Day 145, no respiratory support!
Amazing boy RT!