Head up early.
He had a good night, nurse we have had quite a few times.
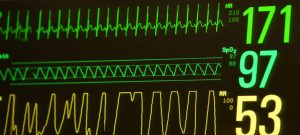
RT is on 25% oxygen!
RT has been sleeping since this nurse got on duty. She has not done cares yet because she us waiting for him to wake up.
Of course RT hears mom and pops voice and starts looking around.
Cares, just pee.
Dr. that is on today comes by to talk.
Says he is planning on going down on flow to 1 LPM today, if we can keep him under 35% oxygen that would be ideal.
Respiratory therapist today is the one that came down from the NICU for his extubation.
We have a good talk, about a bunch of things.
Eventually an order to wean RT’s flow.
A day primary Nurse from NICU comes to visit.
The respiratory therapist swaps RT over to the new low flow system. 1 liter per minute with a goal of staying under 35% oxygen. Really simple, no heater for the air, just air bubbling throug some water to humidify it slightly.
New style nose cannula, looks more comfortable!
RT is doing good on about 25%!
The doctor comes by again, impressed with RT respiratory wise and how everything is going! A talk about when to start trying oral feeds, he is going to follow speech therapists recommended course which is good because that’s what she specializes in.
Feeding is what we need to start working on.
First step is waiting a couple days on this lower flow oxygen, then pulling the ND feeding tube back a little to see if his stomach can handle food in it and him not reflux and aspirate it.
All babys reflux its just a matter of how they deal with it.
With how sensitive RT’s lungs are from everything they have been through, even a little aspiration could cause a large set back.
But when that happened, he had sone things working against him, RT was more premature, had thofalin onboard which can cause the stomach sphincter to dilate, and a cpap with a pressure of 7 trying to force its way into his stomach.
Now much lower flow, almost 0 pressure, full term, no Theofalin.
I roll RT on his side and do some stretches, then his belly some more stretches, he is a happy boy!
Lunch.
Cares.
Occupational therapist stops by we do some more stretches.
Bath time. Mom and I do everything. Clean the important parts, wrinse him off. We put him back because he gets fussy this time, maybe his hernia is hurting. No monitor or sensor to tell us how he is doing during bath time, his color looks good. When we put him back connected. He is sating fine.
Mom’s turn to hold.
It’s nice to be able to pick him up and do cares when we want without assistance, only a few things we are not allowed to do now without help.
Very stablessed day.
Only a 3 or 4 desats, he self recovered. Two drops in his heart rate though during events, not his norm… we will keep an eye on it.
Hang out time.
Cares. Hang out.
Dinner.
Back to PICU.
I hold RT. He is a little fussy.
Shift change, Nurse we have not had yet.
Respiratory therapist tonight is one that we have not had yet.
They don’t have to do much now on low flow though, just check flow and oxygen percent.
Nice and simple.
Hang out. Put RT back.
A night primary Nurse from NICU comes to visit!
Good to see our visitors.
Mom holds and rocks RT to sleep.
Time to go try and get some rest!
Love you little man!