Earlier to the NICU today.
RT is on 22% oxygen!
Primary nurse.
RT’s weight is almost 8 lbs. 7lb 15.4oz.
Morning was slightly more eventful. More events more suctioning. Different vibe around the room.
Two babies are gone, one new admit.
Poop this morning after a suppository.
Primary nurse is definately excited we are going to the PICU.
Hopefully it’s what is right for RT.
I take down his signs.
Morning rounds the doctor asks if we have any questions.
Nope no questions.
It is the doctor that was there for RT’s birth, it’s only fitting we have him for our last day in the NICU too.
Then we prep his crib and head up to the PICU.
Stressful change. New nurses and doctors that don’t know RT and don’t know us. It’s it actually going to be good for his developement?
9th floor.
Different atmosphere, the PICU is only 6 beds but next to PEDS.
Private rooms.
We move RT into his new room.
They swap him into his big bed.
It’s not really a crib anymore.
In his crib he looked big. Now in his bed he looks small again.
The nurse and the respiraroty therapist go out and do passdown to the PICU nurse and respiratory therapist.
The picu doctor comes and talks to us, we voice our concerns with the et tube tape job. Sounds like they will allow the 3 prong method so that RT can still get his binky.
Xray ordered.
After pass down it is time for cares.
The nurse does most everything to get a feel for RT and do a once over I assume.
I notice she suctions too deep and point that out after cares. Not sure if they measure differently here.
She takes my words to heaRT and thanks me for the input. She doesn’t go that deep again.
Xray comes, we step out of the room as per PICU policy. Because somehow standing outside a doorframe the same distance from the xray machine as we would inside the room we will recieve less radiation…. X-ray to me looks good for RT!
After cares we go to lunch. On the way out the doctor is at the desk with our Pulmonologist, they pull it up. X-ray looks good to them too!
After lunch back up to PICU.
He was flailing around while we were gone.
They brought in a white noise machine. It is making a heart beat sounds and they think it helped calm him down.
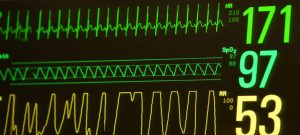
22% still!
One of the march of dimes workers stops by, a NICU manager stops by, a nurse stops by. The PICU chaplain stops by.
An occasional dip in his spo2.into the 70’s most self resolved. A handful of times he gets suctioned.
Another set of cares, this time she let’s us do everything. She is out of the room for a good part of it.
Glad that first care was just for her to get her base line and not the norm.
The Occupational therapist comes and stops by and they do some good stretches.
He is nice and relaxed, swaddled up.
They retape his ET tube, the way with 3 prongs instead of 4. Makes it possible to use his binky again. He gets angry for retape jobs.
I help hold him still. The ET tube slips out about 2 cm. Before they put it in to the correct number before retaping it.
Well no accidental extubation yet….
I give him his binky, he loves it! The nurse has never seen an intubated baby suck on a binky.
Wonder how many intubated babies they have had then. That’s OK, she knows her stuff and is nice in explaining the differences between here and the NICU!
They aren’t too used to NAVA mode here, most of the doctors prefer a different mode.
One of the alarms is PAW high, essentially it means his peak airway pressure is high. It happens when he is angry or bares down or sneezes. Since the rooms are individual they are required to have the vent alarms at 100% volume.
Which is rediculous loud. Turn that amp to 11 loud.
Maybe we can get that turned down slightly.
Another quick set of cares.
Dinner.
Back to PICU.
22% still!
Two NICU respiratory therapists stopped by while we were at dinner.
It’s nice of all our NICU friends to stop by! I hope they keep coming by!
Shift change. Obviously a nurse we have never met.
Another set of cares. Suctioned turned and he his heart rate dips then starts to drop his spo2. 57 it still hasn’t alarmed, I kindly point out his sats are dropping and he might require more oxygen. Bumped up to 100%.
His spo2 keeps coming down.
The respiratory therapist asks the nurse to turn on the ambi bag. It’s for emergency use, kind of like a black bag but not…
Suctioned.
The nurse does not hear her. I prepare to turn it on for her but I see his sats start coming back up.
Low spo2 of 18… Lowest he had gotten in a while now. He turned pale.
They ask if that Is normal for him.
No definately not lately.
After the event back on 22% oxygen.
Maybe he did that occassionaly in the past.
Both the nurse and the respiraroty therapist seem soft spoken.
An ongoing conversation through the cares is that the nurse does not like the tape job of his ET tube. They keep saying it is because the parents want to use the binky.
It is actually because we care about our son and want to not only have negative events happen around his mouth. It’s a miracle he does not have an oral aversion and through hard work. It’s good for his developement as well.
We point out that safety is the biggest concern and if she does not feel like it’s safe then it should be retaped.
Sounds like this is not the norm for her.
She asks if it’s normal for it to be like it is, yes it is, we have had the mustache up until this last couple days and this is the 3 prong with more tape. He has not yanked it out yet.
She seems unsure about the tape job and the respiraroty therapist didn’t instill any confidence.
I’m sure everything will be ok….
Atleast he is back on 22% oxygen.
I’m sure it’s just an awkward position for them to be in. They are used to taping larger children’s et tubes and need as much reinforcement as possible. Probably also not having to be as concerned about aversions to anything near the mouth.
I feel like while picu is supposed to be more developement oriented, this is one area they are less familiar with.
I guess we will see how the other areas are as we move along.
We made it clear if they felt safety was being compromised they should feel free to retape it.
It will be interesting learning each of these nurses styles.
We have another day ahead of us tomorrow so we are going to try and get some rest.
From the reaction we saw i would guess PICU nurses aren’t as used to emergency situations as NICU nurses. I’m hoping we aren’t compromising his safety just by having been moved to PICU.
I either will have to accept RT will be ok in their hands or be there at all times to try and help catch things before they happen. Had I not told them to turn up oxygen yet how much lower could he have gone?…
Overall a good day from a stability standpoint.
99.8% stable day on 22%. They almost acted like there was no knob to adjust his oxygen. For events that they needed oxygen they bump him up to 100% temporarily. Then back to 22%. Not sure if it’s necessary to go that extreme, but ok.
Hopefully no more big events like that.
Please.