Go to the Lytle center to check if they have room to accept donor milk. The process to get mom approved to donate to the Northwest Mothers milk bank finally went through last Thursday. It was a huge screening process to complete. It makes sense though but should not have taken almost 2 months.
Mom works very hard to keep her supply up and have enough to donate and help other preemie babies that have mom’s that don’t have their supply or come in or produce enough!
They tell us to come back in on Thursday. They should have more room for donations then. They only accept 300 ounces per week.
Head up to the NICU.
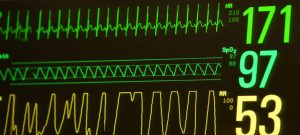
41% oxygen…. Being over 40% makes me verry anxious, when for the last several days he had been under 40.
Dr. Comes by doing morning rounds. They decide to wean his respiration rate by 2.
Primary nurse today, Nurse says she just had to bump him up. Then weans him to 37%.
Nurse mentions there was a surgeon stopping by to look at a different baby for hernia surgery and she had him check RT out because we are intubated and had this question in the past, because surgery requires intubation of we are intubated maybe we can do it early rather than at 50+weeks.
She also asks about G tube placement. A tube that has a valve from his tummy rather than have to go out down his throat or nose. RT may require it if he is not able to bottle feed his compete meals. It’s a more permanent solution.
If they were going to do hernia surgery they could do G surgery at the same time.
The surgeon says that they were not thinking about doing it soon but could do both later on at the same time.
The reason for not doing hernia surgery early on is because its like trying to sew wet toilet paper. They wouldn’t want to do it unless absolutely necessary.
Sounds reasonable, nice of him to check RT out.
Walking in at 41% oxygen how ever brief makes my mind think fast about changes to that can be made.
We do lunch early, skin to skin early today too.
Back up to NICU. I tell the nurse if she sees the Pulmonologist I have some questions for him.
RT is hiding under his swaddle. He likes trying to hide, or maybe he is just trying to get his hands free from the swaddle. Cuter if he is hiding though.
Cares, temp, pee, cpt, suctioned.
Skin to skin.
Down to 27% oxygen for a bit.
RT desats to 84spo2, gets bumped up to 31% oxygen.
Pulmonologist stops by.
I feel like we are in a perpetual loop, we put down the ET tube to get out fluids and help his lungs. The ET tube causes him to create secretions, suctioning causes secretions. We want him to breathe on his own, but we want him sedated so he doesn’t pull out the tube.
We want him to grow and create new healthy lung tissue, but all these things damage lung tissue.
Would it be better to bump up the steroids to be able to wean his ventilator settings faster. But steroids stunt growth…
He says that yes it’s a catch 22. But we are slowly weaning his settings and moving forward. We will get extubated.
He thinks we could drop the respiratory rate again even though we did it this morning.
He also does not necessarily think higher steroids would help at all, he thinks the dose we are on is already being effective, might even be able to wean the steroid too.
Also RT will be growing lung tissue potentially until he is 18.
If higher steroid doses would not help at all then that idea would not work.
He mentions small fluctuations in oxygen percent is more important than keeping him on the lowest possible oxygen although lower is better. Large fluctuations contribute to pulmonary hypertension.
4 hours of skin to skin! Near the end he has to be bumped up to 34%.
Good skin to skin!
Then we do cares, and a bath! Occupational therapist stops by and helps with the bath and does some stretches. After the bath she walks me through how to do a massage that will help with his pooping. Oil up my hands then massage slowly an I on his right side, then an upside down L then a upside down U. 3 or 4 times.
Dinner time.
Back to NICU.
Primary nurse! Asks about G tube discussion. Thinks if we are intubated it might be a good idea. From her experience it is likely he will need one.
Cares. Temp Big poop! 44 grams! Clean him up, Close him up CPT, another poop! One was green the other brown, odd how different they were.
Night rounds, doctor asks if we can stay and have a talk after they are done.
Ofcourse we will be here.
30 minutes later the doctor arrives too discuss G tube and hernia.
Discuss the possibility of needing a G tube. Lots of things working against RT, high probability that he will not be good at feedings.
I voice my concerns.
1. Assuming he has an issue before he has it.
2. Potentially causing other issues with surgery for an issue that does not yet exist.
Dr. Agrees. Normally wouldn’t happen at this point but RT has a high chance of needing it.
3. Putting unnecessary holes in him is just a way to introduce infection. We already know he likely has a compromised immune system because heit’s premature.
Dr. agrees but it’s a low risk.
4. We are assuming that reflux was a large contributing factor in why he was intubated a G tube goes into his stomach and then we are having the same issue as before and going to be reintubated anyways.
There is another option that doesn’t go into the stomach but to the same place as his ND tube. But often done at an older age.
5. Bottle feeds are a ways off, if they don’t want to do hernia surgery yet then we have to be intubated again anyways.we will hopefully know by that point more on if he will actually need to have a G tube.
Surgeons will have to weigh in on what age the surgery can be done for a high success rate.
It will be an ongoing discussion.
I then bring up the respiratory plan and the questions I discussed with the pulmanologist today.
This Dr. As do some other ones have a different stance on steroids and believes it would help get off the vent faster.
I give the doctor my stance. Hopefully whatever course we take it is the correct one. No one knows. If it’s the way I want, and it goes poorly then I will feel guilt. If it goes the other way and doesn’t work it will be an I told you so moment. Which is frustrating being that they have more knowledge and experience.
If either way goes well. I will be grateful.
Interesting the vastly different ideas on what is the correct way to move forward.
How fast we move kind of depends on the surgeons response on when they can effectively do the surgery and not have to do revisions on it.
Long discussion condensed into several sentences. It will continue to be ongoing obviously.
RT has a larger event during the end of the conversation needs lots of suctioning, almost needs to be bagged but comes back up.
After he is all settled down its time for us to say our goodnights and try and get some sleep.
Love you clever boy.