The primary we should have had today is sitting at the front desk. She has been reassigned to admit duty today.
RT has a nurse that has never had him. I guess the whole asking for nurses that have had him to keep continuity of care has been pushed to the back burner.
Atleast he has had mostly stable days.
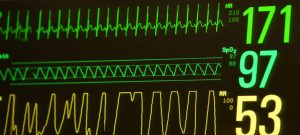
His oxygen percent is on 55%…
His IV lines have been pulled.
Fentanyl is stopped. Just on oral morphine now.
The nurse apologizes for being a new face, she says it’s probably our worst nightmare having nurses we have not had.
Not close to the worst nightmare… but definitely more stressful, RT has a long history, its not really possible to pass everything down without missing some important stuff.
Only two events last night. Glad he had another stable night.
Getting frustrated that we are creeping up on oxygen needs. When he was intubated he was on 21% for several hours. We are more than double that and continuing to trend in the wrong direction.
At 1400 cares during repositioning he works some secretions loose. Large event, heart rate into the 50’s. Spo2 to 10 and then low enough to not read several times.
Code alarm eventually pulled.
He recovers before everyone arrives. 100% spo2 before the doctor arrives.
They turn off the alarm.
Doctor asks what happened. Someone that just arrives says he didn’t like being suctioned.
I correct them and I say no. Movement and working secretions loose. He likes the suctioning if we didn’t get it out he would still be being bagged.
Why would someone that does not know RT, and was not present for most of the event try and inform the doctor?
It just makes everything more confusing.
I hear someone out in the hall say “it’s just (insert last name) being (last name)”
Yea lovely.
It’s not even his fault that he can’t get out these secretions on his own.
After the event he is on 53%.
Temp, Diaper change, Skin to skin time for me.
They bump up his oxygen for the transfer, it goes smooth.
He is relaxed because of the morphine.
He opens his eyes though and looks at me.
The respiratory therapist and nurse leave. I ask the wife what they bumped his oxygen up to for the transfer.
She says you won’t be happy with it.
71% oxygen…
Is anyone else even concerned? Skin to skin is supposed to help him.
Why am I even doing this.
He obviously likes being on us but he doesn’t need to be on 71% oxygen. If he does then there is other issues going on.
Eventally he gets weaned. I ask what he was weaned to. 70%. Ok weaned by one. We will get no where.
How is this ok?
Why has there not been another xray recently to see how his lungs are?
4 and a half hours later the end of skin to skin we are weaned down to 50% oxygen.
Bumped up 6% to transfer back to his bed. 56%. That’s better, don’t need to bump up 20%.
Shift change. At least we are having a nurse in nights consecutively same one as the last few nights!
We have a talk with tonight’s respiratory therapist and nurse. Discuss X-ray not being recent and higher oxygen, needs trending up. Respiratory therapist talks to the doctor. Xray ordered for tonight!
2000 temp, diaper. Repositioned.
Already weaned to 50%.
We need a stable night!
Love you little man!