We stayed the night in the parent sleep room on the 2nd floor to be just a little bit closer. It is a good feeling to stay close afer a rough day. Not better sleep, because it’s a slightly worse and smaller bed than at the hotel but it is worth it to be closer. Made possible through donations! Hopefully someday I will be able to donate to do something like this.
In the morning I am jarred awake by a fire alarm. I quickly throw on my clothes, grab my camera backpack and phone charger.
I wonder what they do in the event of a fire in the NICU 4 floors above me….
I exit the sleep room and go to the nurses station in the hall.
Thankfully it is just a drill.
That’s one way to start the day. I head up to the NICU, wife is having breakfast with a friend. They will meet me up there in a bit.
I enter room one. There are about 8 people infront of his bed.
Turns out they are talking about the baby across from ours.
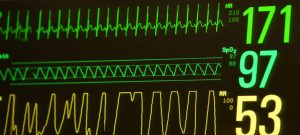
RT is at 60% oxygen though, when we left last night he was down to 27%…
Respiratory rate is set to 35, tidal volume 30.
Nurse today has had him quite a few times!
Turns out he had a mellow night, around 30% oxygen. But around shift change at 0700 he started requiring more. Probably because it is brighter, and louder.
He also had a larger event and took a while to come up. They ordered a chest xray. An order for albuterol to help stop bronchial spasms if he is having any.
Xray shows up quick, Xray shows the ET tube slightly deep, they pull it out a little, hopefully this helps. Another xray, placement looks better.
Albuterol given, able to wean his oxygen down to 45%. Blood gas ordered for in a little bit.
Blood gas is good.
Temps have been stable, just pee since early yesterday morning. Probably saving up poop due to stress, fluid restriction, and being NPO from 0800 yesterday.
1100 first feed. Starting small and then ramping up as he tolerates. Some discussion of when to extubate.
He is more awake than last night but still not very. Still on fentanol with tylenol as needed, hopefully going to just go to tylenol as needed.
Eye drops every 2hrs to keep his eye muscles relaxed, another every 6 to reduce swelling.
The rest of the day is relatively uneventful, we spend just hanging out bedside. Normal temps, just pee. Stressing about why his oxygen needs are higher. His heart rate dips below 100 from 150 occasionally when he wakes up more and realizes he had a tube down his throat. He bears down to try and push it out which is ofcourse unsuccessful.
He is more aware now than he was two weeks ago. He also knows he doesn’t have to have a tube down his throat. It definately upsets him and causes him some stress.
Around 1700 while talking to him he smiles some and tries to open his eyes for the first time since surgery. He gets then barely a squint open to look at us. Mostly we are keeping his face covered to protect it from any lights that may get turned on.
1900, shift change, primary nurse tonight! 40% oxygen
RT definately hates being Intubated. Some talk with dr at night rounds about extubation tomorrow. I ask if we can do nava mode before then to ensure he is ready and he likes that mode more so he should do better. Dr. Agrees. Hoping he does well through the night and be able to extubate and go to CPAP tomorrow.
2000 cares still just pee. Albuterol every 6 hours. Flow vent evry 6 too. Suctioned. Turned. Feed. He has been bearing down and desating, maybe he is constipated.
2200 swap to NAVA, EDI catheter placed. Trainee helps swap him over. He seems to llike it. Nava level is tried at 1.8 what he was on when he was extubated. Turned up to 2.0. That’s OK. Good spot to start.
Apnea alarm set to two seconds to start with.
Sapository to help him poop.
He settles down to 30% oxygen. Much better. Edi signal is showing pretty good activity!
Hopefully able to make him happy and extubate tomorrow!
Keep up the amazing work RT!
Shorter post with not all events through the day. Tired. Time to get some rest.
Short, but happy moments are what keep RT wanting to stay in this world, it is our job to give them to him.
Seeing him flash us smiles throughout the day during milk swabs, feedings, hand hugs, and just talking to him, tells us we are doing the correct things and makes it all worth it.