Wife wakes up early to pump.
Phone rings, it’s the the hospital. Did he have a big event? Is he ok? Did he yank his tube out on his own last night? Did he regurgitate some food and aspirate it again? Maybe he is just angry and they are telling me so I can come in and try and comfort him. Just a few of the many ideas that run through my head in the second between my phone ringing and me answering.
Hello, this is Dr.
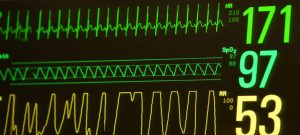
Dr: RT is ok. I just wanted to let you know we are not planning on extubation this morning because he has been on back up mode 80% of the night, normally 15% to 17%. He also got irritable for about an hour, and had a high temp. Worried about infection, doing lab work to check white blood count and a culture. Don’t want to attempt extubation if we have other things going on or things that would really be working against us.
I ask what percent oxygen he was on during the night.
27-32%.
Me: one thing I have noticed is now that he is able to breathe on lower oxygen if he is turned up he likes to ride the vent to not high sat on his spo2. Then if you turn him down, he will work more to breathe when his spo2 goes down.
Dr.: Oh… huh. Interesting.
Me: Yea it seems like he is getting good at self regulating his spo2.
Me: What time do you think it would happen if it does today, or would it just be depending on RT and how he is doing?
Dr.: Yup that one, but my guess would be no earlier than 1100 now. I didn’t want to scare you but, I just figured you would want to know. Before you showed up this morning.
(She is correct)
Me: yes thanks for the phone call Dr. Heve a good day!
I will try and get a little bit more sleep then before we head in. Mom already drank coffee though and was ready to heat up. Now she won’t be able to get in a nap.
Short nap, then up to NICU for the day.
We arrive, labs have been sent off for blood culture and wbc.
RT is looking fine, on 23% oxygen now!
Weight on the board is
The respiratory technician is there looking at him checking the EDI catheter,
She explains the reason for no extubation.
I mention what I said about how I have been seeing the lower the oxygen percent the harder he will work and be in less back up mode. If his oxygen percent is lower he rides the vent less and has to breathe to keep his spo2 up.
She says she doesn’t think that’s what this is.
Eventually the Oncoming Dr. Comes by for morning rounds. They talk about extubation and why we haven’t done it yet because of worry of infection and how much he has been in backup mode, he says as soon as the labs come back he plans to extubate. He isn’t concerned about the percent he has bedn in backup, he uses more docterly words to explain what I have noticed about him riding the ventilator.
He says the portion of his brain that senses spo2 and tells our body to breathe is telling him he doesn’t have to breathe because he is over ventilated on back up mode, so it’s not that he is forgetting, it’s that if he did breathe more than he was being forced to his spo2 would go into an unhealthy high range.
Alright! Good to hear the Dr. Believes RT is actually not breathing because it’s better for him. Glad to hear he thinks there is nothing wrong that would point at no extubation as of now.
Extubation is back on for today!
We do cares, just pee. Temp is slightly high, his inguinal hernia is looking worse. Everything is more pushed out. It doesn’t look comfortable. The nurse checks it out, firm but still not too firm, no discoloration. It looks worse than it ever has for me in the past.
Eventually it is time for the nurse and respiratory therapists to prep for extubation.
I go and get my camera from the locker.
They get everything ready, swap him to the back up breathing machine called neopuff to change the settings to NIV NAVA.
Both of these respiratory therapists know him pretty well. They ask if I’m ready to take some pictures, they are ready to extubate. Tape is removed! He is turned up to 40% oxygen.
Put on a hat that his NIV NAVA will strap into
One last breath while intubated, then it is removed. His little face is free of tubes for a little! I get a video and some pictures. They swap in a little face mask.
Our boy is extubated!
The respiratory therapists strap the mask into his hat, and start to fiddle with his settings on the ventilator.
Eventually settling on a Peep of 9 (which is quite high), NAVA level 3.8 back up rate of 40. Back up pip of 27.
He seems to be doing good, oxygen percent turned down to 30, then 27, 25 and eventually to 23%, then 21%.
He seems to be handling everything fairly well. Kind of a little freaked out by the air leaking out of his mouth.
NIV NAVA works by keeping a positive pressure (peep) to have his airways inflated then higher peaks in pressure (pip) for breaths. The Edi catheter is down his throat ending in his stomach it picks up the signals his brain sends to his diaphragm and assists with giving a breath based on the strength of the signal sent. Obviously pressure wants to escape to the path of least resistance, which in this case is his open mouth. We have higher peep so that atleast some of the pressure makes it down his airways rather than in his nose and out his mouth.
Some air can also make its way into his stomach so it is important to vent the OG (feeding tube) tube to allow the air to escape from his tummy.
If he opens his mouth a larger amount of air escapes through his mouth, causing wet snoring sounds, which upset him and probably feel weird, which cause him try and yell, which cause a larger leak and more sounds, it is kind of a vicious circle, he will probably get used to it, and hopefully get better at closing his mouth. If it becomes too much of a problem they have a chin strap.
They want to try and not use the chin strap if possible because of how high his peep is set, don’t want to over inflate his lungs more and cause damage. Also if he regurgitates it won’t be as easy for him to cough it out.
They position him to his belly head facing the right side and swaddle him, he looks agitated and can’t get away from the tubes infront of his face or the sound coming from his mouth. They watch and he picks up his head and turns tubes going under his lifted head almost facing the opposite direction. .. they try and help by reposting him facing the other way so he is more comfy. But the tubes are still right in his face and the sounds coming from his mouth so he again turns the other way. They reposition him so he should be comfy. Silly RT.
Then he picks up his head yet again this time he stops with his face straight down his little nose mask buried into the his bedding. When he is here the bed holds his mouth shut and stops the sound. What a silly but clever boy, the nurse and respiratory therapist laugh, they have never seen centerline prone as a position before. RT is quite the independent little man. He calms down almost immediately in this position.
Quite the impressive muscles he has, not only is he lifting his head, but his mask and tubes. He shouldent even really be having to lift his head at this age yet.
Back up to 23% oxygen then 25% back down to 23%
Eventually we head to lunch in the cafeteria, I get a small piece of cake and a coffee to share with the wife in celebration of RT’s successful extubation!
Then back up to the NICU, he is still at 23%! He behaved while we were gone.
1400 cares, temp 37.6 nurse turns incubator temp down. Inguinal hernia looks maybe slightly larger, just pee in his diaper.
1600 larger event, we think becausehe had his mouth open and not enough pressure down to his lungs he was 56 spo2. Nurse turns up his oxygen 37%. Nurse has the neopuff at the ready but he works his way back up.
It is more nerve wracking watching this event while he isn’t extubated. I feel like it would be harder to get excretions out if he isn’t breathing. There is no tube down his throat holding his airways open or a catheter that goes down there.
He just has to cough out the secretions and drool or have a nurse suction out his mouth. Which he needs frequently.
She turns him down to 32% after he levels out.
1700 cares, just pee, hernia looks the same. They want to give his face a rest every few hours from the mask so swap top nasal canula. He hates having prongs in his nose. We have created one angry baby by sticing tubes in his face and little things up his nose. Lots of sound coming out of his mouth. Heart rate gets 220 the respiratory therapist gets a binky and cuts a portion off the top so it fits with his tubes on his nose. He takes it in his mouth sucks a little then pushers it out. He calms down briefly but does not like what is happening. Try hand hugs and milk swab, these things calm temporarily but he is upset. Swap back to the face mask and he calms down slowly.
1830 work up the courage to go to dinner at the hotel’s restaurant. Then back to NICU.
Shift change has happened, one of his primary nurses is back on tonight!
He is at 27%.
2000 Time for cares, just pee, hernia looks worse to me. Nurse checks it out. She says it’s still not too hard. Swap to nasal cannula again to try it out, a smaller size this time. Same issues as last time but not quite as angry. He enjoys his binky this time. Some milk swabs too! Eventally he settles slightly, but when I pull my hands out of the incubator or stop holding the binky in his mouth he gets upset again. Several rounds of doing this and he seems to eventually calm down and stay more relaxed.
Huge day! A successful one! He is extubated! This is a big step in the right direction. Hopefully his lungs will continue to grow stronger fairly quick and we can wean down his PEEP, and settings. Eventually the next step will be a move to CPAP! (Constant pressure to hold airway open he does all the breathing on his own. No back up mode.)
It is nice to see his face without as much tape, such a cute little boy we have!
I’ll try and post photos tomorrow!
Keep growing and going!
Go RT!