Weight in the board, 1655 Up 5 grams.
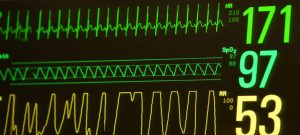
Oxygen percent still sitting at 53%.
They have a checklist out for another blood transfusion, we were guessing this would happen today after Sunday night labs. Last Sunday his red blood cell count was 29.8 that was before surgery and countless attempts at IV, picc line sticks, blood gas, and surgery. Now it is down to 26.
A new murse for RT, it is the first time RT has had a male nurse! He tells us the Dr. Today discontinued the Albuterol that was started yesterday, likely starting up the strong steroids again after blood transfusion to help reduce swelling, then the Dr. Wants to try and extubate in the next few days. We ask if it is the Dr. That tried it the first time. It is. We kind of laugh. We figured he would be the next one to try again after surgery. He is forward thinking.
Morphine weaned by half again. Now only .04 every 6 hours. He
1100 cares just pee. He had a couple smaller poops over the night. Respiratory therapist repositions him and suctions and gets large amounts of secretions.
Eventually the blood arrives, his new IV is already in. Transfusion started no more feeding till 2300.
A few of the people that are more familiar with us come by, we get more welcome backs and big waves, it feels good to see they all care.
Quick lunch then back to NICU.
Dr. Comes by, we talk about the plan mooving forward, he wants to try and extubate a day or so after starting the dexamethazone back up for the best chances of success. He wants us ideally in the 30% oxygen but thinks we can succeed in the 40%. Either NIV NAVA or CPAP. Two different non invasive modes of ventilation. Likely higher peep to hold his airways open. He says some Dr. Might not feel as comfortable or daring as he is with that high of a PEEP but he is confident RT can handle it without rupturing a lung…
They change his ventilator settings slightly, inspire time increased by .10
As he gets his blood transfusion we are able to wean his oxygen percent more.
1400 We do another care, he tolerates it well. He pooped! A decent size too!
Down to 48% oxygen after cares mom gives him some hand hugs and talks to him. He is a happy boy, mom gets some smiles!
1530 blood transfusion complete down to 45% oxygen. He is liking his blood and being able to transport those oxygen a bit better. He probably now has the highest red blood count he has had since before surgery.
1700, just pee for cares. Temp is a little low. Bumped up temp in his incubator. Repositioned, suctioned, not much excretions.
Dexamethazone meication started, Looks like a larger leak on his ventilator tube in this position, or Dex is working and being a bronchial dilator.
Up to 47% oxygen. Shift change, new nurse that has not had him before.
2000 time for cares, just pee, mom cleans his eyes. The nurse repositions him with the respiratory therapist, the respiratory therapist bumps his oxygen up from 47% to 60%. For all his previous cares today he didn’t need to be turned up. She did it preemptively. RT is arching his back trying to get away from the ventilator tubes. He is really angry. The respiratory therapist positions his tubes, they look really awkward and kind of curled up and spring loaded. She makes another small adjustment and one of the tubes disconnects. It takes several tries to get it reconnected because it is awkwardky curled up and comes tight before it reaches. Maybe it should not be positioned this way. His head is tilted back not inline with the rest of his body. She suctions him out and doesn’t get much. He is angry, lower lip quivering mad. His heart rate hits 217.
They tuck him in and swaddle him, he doesn’t want to calm down. The respiratory therapist asks if the nurse needs anything else. Nope. Respiratory therapist goes off to help another baby.
I go around infront of RT, oxygen percent still sitting at 60%. He is crying and upset. The lock on his ET tube is poking into his mouth, his neck is tilted backwards away from the tubes.
Mom and I try and comfort him, I point out to the nurse what is happening and tell her he is picky with the tube placement, and how tilted back his head is. She pages the respiratory therapist to come back and adjust the tube. She doesn’t want to uncurl the tubes from the way they are or reposition his head, but kindly adjusts the lock out of his mouth. He is happier but still uncomfortable because of his neck. She asks if that is better, I agree and thank her for adjusting it even though it’s not exactly what I wanted done, off she goes.
We try and calm him down but it isnt working so I ask the nurse if we can rotate his body so it’s in line with the tubes and his head won’t be tilted backward, this way we don’t have to mess with them if she isn’t comfortable adjusting them.
I don’t think I’m actually allowed to adjust his tubes for liability reasons but I’m not sure. She kindly says she would rather not mess with the tubes but will get another respiratory therapist. She pulls one aside and he graciously comes over, mom and respiratory therapist adjust RT til his head is not tilted back and the ventilator tubes are not spring loaded.
This looks much better! We don’t need him getting accidentally disconnected again.
We reswaddle him and he calms down quickly. Ahhhh finally comfy.
I’m disappointed that I feel like we had to explain how to make him comfy. Most people understand he is sensitive and doesn’t want his neck bent backwards, maybe some babies would be ok with that?
The nurse thanked us for being awesome parents and reminded us we know him better than anyone. It is nice that she values our input and got us help when we needed it! Hopefully she can advocate for his positioning in the future!
The nurse is able to turn his oxygen percent down 50% now. Hopefully she will be able to wean him more before the next care.
Nurse is able to get him down to 45% oxygen for a little bit!
2300 47 percent for cares. Big poop! Almost a blow out! Theofalin started back up, feeds restarted to full feeds of 28cc and fortified with 24 cal HMF after the NPO because of blood transfusion.
Have a good night little buddy! We love you!