1700 shift change, the primary nurse he had last night is back.
Sounds like the nurse we had today and yesterday should be back tomorrow!
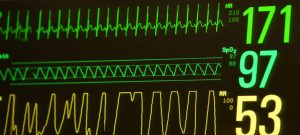
He does well with passdown only gets one extra percent as a bribe. He only has a couple brief desats to 87 spo2.
Time for cares, temp check, he is slightly warm now 37.4 we overshot his temp slightly. That’s OK he will cool off during cares slightly.
Some pee in his diaper. We a apply an ointment Nystatin (anti fungal)to his bits to combat any possible yeast infections.
Then respiraroty therapists suctions him out and does CPT (chest physical therapy (vibration)) it helps break up the fluid for easier suctioning. Some good secretions come out. Respiratory therapist says he sounds much better than yesterday.
His head measurement has increased by .3 cm. Could just be his swelling fluctuations. His head does look puffier today.
Dr. comes by bedside for night rounds. Nurse mentions his increase in head circumference, Dr will likely order a cranial ultrasound for tomorrow. Dr. Has had a busy day attending to other babies, today RT did not have to be his focus!
It sounds like we have some progress on surgery plans. Likely to do it at Mary Bridge. It sounds like they focus more on preemies while seattle children’s focus is more on full term babies. It is the same surgeon at both locations.
He has continued to be stable for most of the day. We are going to get to do iur first skin to skin in two weeks. We are grateful he is stable enough to do this, skin to skin is an important part of the process to make RT healthier.
The Respiratory therapist goes and talks to the Dr. she comes back a short while later.
She tells us Mary Bridge uses a different type of ventilator setting and she wants to transfer him to it tonight to see how he does on it.
The doctor agreed. We will swap him from pressure control to PRVC. We will do this after swapped to mom and his feed is done so not all at the same time. It’s good to not do everything at once that way you can better diagnose if one thing is causing issues.
2100 Standing transfer goes smoothly. Mom picks RT up, bends forward and holds him to her chest, respiratory therapist helps guide his ventilator tubes. The nurse wrangles all of the dangly IV lines. Mom moves smoothly and slowly sits, we position the chair so nothing will come tight and recline her to a comfy position. RT is doing well. CPT on his back and suctioned again.
Time for food RT! 20 CC now! 30 minute later the food is in.
A short bit later the respiraroty therapist is back. She swaps him to the new mode adjusts some settings and seems to find a happy place. Slowly begins to wean his oxygen. He controlls how big the volume on his breaths are in this mode. Pip of 22 depending on how big his breaths are, Peep of 8 to hold his lungs open and not allow them to fully collapse. Respiratory rate 40.
Eventually she has him down to 36% oxygen. This looks like it’s working good to me!
I take his temp, holding good 37.2.
RT is liking his mommy skin to skin time and the new breathing mode!
Hopefully we don’t lose any lung recruitment.
2200 nurse does a blood gas, looks pretty good, co2 level is staring to come down 38 now, might end up weaning something, but good for now.
2345 comes and it’s time to put RT back in his incubator. The respiratory therapist suctions him before moving him to try ans ensure the same thing from the other night doesn’t happen during repositioning…
The transition into the bed goes fairly smoothly, but then he realized he was no longer on mom. His numbets started dropping across the board. Heart rate dipped to low hundreds. Spo2 follows as it tends to do. Respiratory therapist suctions him a few times and gets lots out, nurse suctions his mouth out, lots of sticky thick secretions. His drool on the side of his face has made a sticky gummy substance, maybe some of the adhesive from the tape on his face softened? Hopefully none of this made it into his mouth.
His oxygen is turned up to 100% spo2 only gets down to 64.
These two are are quite the team.
The respiratory therapist brings in another person to bag him while she suctions. They get out some more large amounts of secretions. His sp02 hits 100.
They turn his oxygen down a little but he doesn’t tolerate it well. Back to 100%
0040 heart rate hits 202. He is really angry he isn’t on mom anymore. He also has probably realized how much more work he is doing to breathe on this new ventilator mode.he was just so comfy on mom he didn’t notice
Well we almost had a really stable day.
As his heart rate comes down they are able to turn his oxygen percent down.
0127 still weaning his oxygen percent. Down to 70% now. He seems relatively stable just agitated and requiring more oxygen…. did anything else change? I wonder what this mornings xray will show.
Feeling really happy I have a 0730 appointment with DEERS at base Seattle to redo what should have been done on wednesday.
At some point we will have to decide to get some sleep for ourselves.
0210 he is at 63% still stable. Looks like he is finally asleep.
Going to head back to the hotel and try and get a few hours of sleep before it’s time to pump and go to our appointment.
He is in good hands.
Sleep tight little guy. We love you more than anything.