I’ll start the post with the best news of the day… He pooped for my last diaper change of the day!
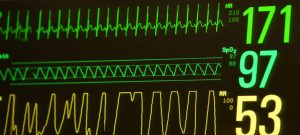
Enter NICU, oxygen is at 58%. Alright we will take it. Weight on the board is 1380 a loss of 10 grams. To be expected, just TPN fluids and emulsified lipids, while getting rid of swelling.
The nurse on today is one of the first ones to have him when he was born, she was the first nurse to make him a poster too!
She asks how we are holding up, then tells us how RT has been doing and the Dr.’s plan for the day.
Dr. Today Is the one that was there the day RT decided to come.
Echo cardiogram scheduled for 1400, to re-evaluate for heart surgery.
Dr. Is wanting to try and get him off of oscillator and back onto SIMV mode on a conventional ventilator.
He believes the conventional will be better for him and that it will help him strengthen his lungs rather than have his lungs and diaphragm essentially hold in the same position.
I asked this question when we first went to the oscillator. I was told it would not weaken his lungs from not allowing him to move them. Maybe it was planned that he would only be on the oscillator for a few days not weeks? And the answer was assuming only a few days on the oscillator?
Now I have been given two completely opposite answers to the exact same question. Oh well. Two tools to provide different benefits, time to try a new tool to keep progression.
1400 cares, temp, diaper change. Tiny smear of poo. Good amount of pee.
During suctioning they have to turn off the alarms on the oscillator, pause the oscillations and then suction. During this whole process the MAP (pressure) drop off down to 1.1, then 0. The respiratory tech finishes suctioning. His sp02 is still bouncing 99-100. The nurse unpauses the oscillator, and turns back on alarms… Pressure still sitting at 0….. His sp02 begins to come down, 90, 86, several more moments and button cycles and an eternity later and the machine finally comes back to life. 85 sp02, then he starts coming back up.
Then time for echo cardiogram.
I hold his hand and contain him as he gets the ultrasound probe rubbed around on his chest. He doesn’t like ultrasounds.
Then the it’s time to switch ventilators. The Dr. switches him to a bag and breathes for RT for a long time to figure out and feel what settings his lungs should like on conventional ventilation. They bring in the other ventilator he has been on, we will be going to SIMV mode again, Dr. tells the respiratory therapist what settings to enter on the machine. RT keeps his eyes open for all of this to watch what’s going on. He seems to like the Dr. doing the breathing for him. He looks more relaxed.
They hook it up and swap him over. Not all the hoses are connected. RT doesn’t have any pressure or breathing for close to 10 seconds while they figure out what isn’t connected. They finally connect him what feels like an eternity later. He recovers quick.
What a relief. They make a few more adjustments.
His mom notices a hissing of leaking air. We discover one of the air pressure lines connecting the ventilator to the wall has a small leak. The nurse tells the respiratory therapist. She says yes that sometimes happens. It will likely get worse if she tightens it…
I ask if this could be problematic, and cause issues with oxygen percent adjustment. Or if leak gets worse it will cause issues.
Respiratory therapist says it shouldn’t.
It shouldn’t.
I say “many things that shouldn’t happen, have happened.”
I feel like “should not have happened” is a trend.
Is it paranoia when you have a fear of things that shouldn’t happen but happen anyways?
RT shouldn’t have had to come early, shouldent have had a PDA, the medication should have closed it. The antibiotics should have gotten rid of his infection after a 21 day treatment. He shouldn’t have been disconnected from his ventilator by accident and had his lungs collapse. Being disconnected so temporarily should not have affected him so detrimentally. He should have recovered faster. I’m not sure if I should trust shoulds.
But I understand. At least the leak is on the air line not the oxygen line…
Shouldn’t matter.
RT seems to be tolerating the transfer over well. 66% oxygen. He looks stable.
Suctioned a large amount of secretions out.
1600 Time for a blood gas. Ph a little high 7.53. c02 down to 32.
Time for a late lunch, early dinner.
Then back to NICU.
It’s definitely quieter without the oscillator. Although The leaking hose is still quietly Hissing away… I’ll get over it.
We talk to Dr. echo cardiogram shows his PDA is still large amount open and likely continuing to be a large contributing factor to his poor lung condition.
Cardiologist from children’s likely come bedside later today to evaluate him for heart surgery.
If heart surgery is what it takes to progress this is what we will do.
Another blood gas, almost the same. Begin weaning settings.
Pip down to 36 from 37, respiration rate down to 30 from 35. Peep up to 8 from 7.
Oxygen percent slowly coming down!
Cardiologist comes by, he looks RT over, listens to his heart. We have a discussion of how heart surgery would go. Cardiologist calls pda moderately open not largely open. Likely RT will have to be transported to children’s hospital for the operating room.
They will have to do an incision from under his left arm to about the center of his back, spread his ribs open, carefully push his lungs out-of-the-way, identify the right portion of his tiny heart and clamp it off, put everything back and close him up. As you can imagine some risks are involved. He lists off a few of them. Most of them are quite scary.
He believes RT is a good candidate for the surgery but is not sure the surgeons will readily agree.
Open chest surgery, but not open heart.
1900 52% oxygen. We have been able to wean down for a bit now!
Shift change and pass down. RT’s primary is back tonight for her last night till she goes on maternity leave, she will be missed. Big sigh.
2100 weaned down to 46% before cares! Nurse does a blood gas, he doesn’t get very upset, and we start cares.
I start changing his diaper. There is poop!!!!
So happy my boy has finally pooped again! His bowls are trying to start working! Even though he has not had food in over a day! Not a big poop but its a start! Good amount of pee too! Diaper change goes smoothly.
The nurse shows the blood gas to the Dr.
Good job nurses and RT! Some settings are to be weaned. Peep remains 8. Pip down to 34 from from 36. Respiratory rate down to 25 from 30. His co2 is coming down lower, respiratory rate coming down should help it level out. His pH is holding about even.
Time to weigh him!
Suctioned turned and suctioned again, he is calm and we see a few pink spikes on his breathing monitor, meaning he actually initiated the breath! It’s been a while since he has been able to do this, hopefully he gets the hang of it again.
Slowly they wean his oxygen % down as he high sats.. Fingers crossed keep it steady.
We will have an early morning tomorrow. We have to try and package up a bunch of milk, and send it back to Alaska with a friend that is flying. We are grateful of the chance to ship about 40 days worth of milking back home.
Hopefully RT and the nurses get some rest.
0013 Time for us to try and do the same.
Sleep tight my handsome boy!